August 20, 2019
In a new study of seven people with Parkinson’s disease, Johns Hopkins Medicine researchers report evidence that deep brain stimulation using electrical impulses jumpstarts the nerve cells that produce the chemical messenger dopamine to reduce tremors and muscle rigidity that are the hallmark of Parkinson’s disease, and increases feelings of well-being.
“While deep brain stimulation has been used for treating Parkinson’s disease for more than three decades, the mechanism of action is not fully understood,” says Gwenn Smith, Ph.D., Richman professor of psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine, and a member of the research team. “Our study is the first to show in human subjects with Parkinson’s disease that deep brain stimulation may increase dopamine levels in the brain, which could be part of the reason why these people experience an improvement in their symptoms.”
Their findings are reported in the April issue of Parkinsonism and Related Disorders.
Parkinson’s disease is a neurodegenerative disease that affects an estimated 10 million people worldwide and strikes about 50,000 Americans each year, most of them over 50 years of age, according to the National Institutes of Health. The disease is caused by the progressive death of nerve cells that produce the neurotransmitter dopamine. Symptoms generally worsen over time, affecting both movement and mental health.
Deep brain stimulation is usually the next line of treatment when dopamine-enhancing medications, such as levodopa, fail to relieve Parkinson’s symptoms. In a procedure similar to inserting a heart pacemaker, surgeons implant wires connected to an electrical current source, and in a controlled fashion, send tiny jolts of electricity through brain tissue to change how nerve cells fire. Typically, to treat Parkinson’s disease, electrical current is passed in brain areas that receive chemical messages from dopamine-producing cells, rather than the dopamine-producing cells themselves.
Much of what is known about how electrical stimulation changes brain activity in patients with Parkinson’s disease has come from positron emission tomography, or PET imaging. PET scans detect signals coming from radioactive tracers that are bound to specific molecules in the body. Previous PET imaging studies using a tracer for glucose show an increase in brain metabolism after electrical stimulation, indicating a return to a more normal brain activity after the treatment. However, PET studies using a tracer that binds to target sites, or receptors, on dopamine-receiving cells showed no change in dopamine levels after electrical stimulation, suggesting that dopamine may not play a role in improving brain activity and, by extension, easing Parkinson’s disease symptoms.
However, scientists suspect that dopamine might still play a key role in the success of deep brain stimulation.
“We knew that dopamine-producing cells get connections from many parts of the brain,” says Kelly Mills, M.D., M.H.S., assistant professor of neurology at the Johns Hopkins University School of Medicine. “So, even if dopamine-producing cells are not activated directly, electrically stimulating other parts of the brain, particularly those that receive information from dopamine-producing cells, can indirectly increase dopamine production, but supporting evidence in patients was generally lacking.”
To study the change in dopamine levels after deep brain stimulation more precisely, the researchers went in search of other ways to track this chemical messenger in the brain. Of the many molecules that dopamine interacts with, a protein called vesicular monoamine transporter, VMAT2, caught the researchers’ attention. VMAT2 catches free-floating dopamine molecules and packs them into biological cargo bags called vesicles heading towards nerve terminals to release their content.
PET scans of VMAT2 on Parkinson’s disease patients taking dopamine-increasing medications, such as levodopa, show that brain dopamine and VMAT2 are related to each other: As dopamine levels in the brain go up with levodopa, VMAT2 levels go down, and vice versa.
Share Fast Facts
.@HopkinsMedicine researchers show that changes in brain dopamine may be why deep brain stimulation eases Parkinson’s disease symptoms. Click to Tweet
.@HopkinsMedicine researchers may have solved a 30-year-old mystery of why deep brain stimulation improves symptoms of Parkinson’s disease. Click to Tweet
To investigate if deep brain stimulation increases dopamine, the researchers performed PET scans of patients with Parkinson’s disease using a tracer for VMAT2. They also performed PET scans using a tracer for glucose to measure changes in brain activity after the intervention. The study included three white women and four white men, ages 60–74. These patients received PET scans before deep brain stimulation and then after. In addition, the researchers evaluated the patients’ motor symptoms using the Movement Disorder Society Rating Scale and psychological symptoms using a battery of tests including the Hamilton Depression Rating Scale and Neuropsychiatric Inventory before and after electrical stimulation. Trained psychometricians assessed the cognitive abilities of the patients before and after deep brain stimulation.
As expected, the researchers found that after deep brain stimulation, Parkinson’s patients had considerably fewer tremors and less rigidity. In addition, the patients also showed improvement in cognitive abilities and mood, with depression scores lowering by as much as 40%.
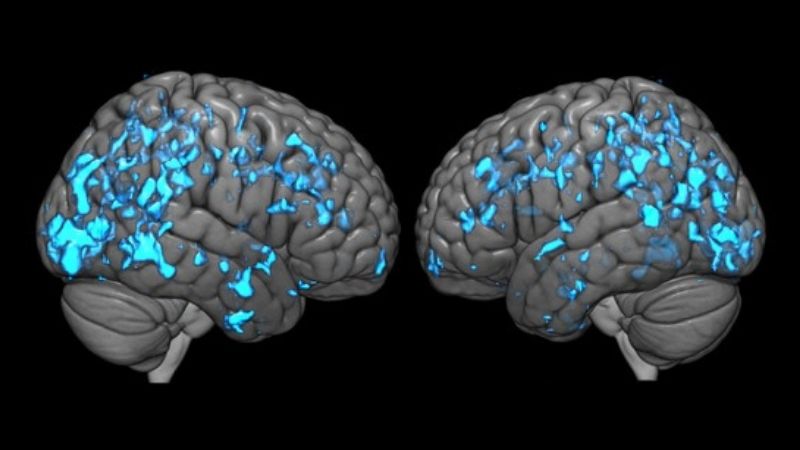
Analyzing PET scans, researchers saw that after deep brain stimulation, all seven patients had lower levels of VMAT2, implying that there was an increase in dopamine levels in the brain. The PET scans for glucose showed that after electrical stimulation, brain activity in these patients had improved in areas that coordinate movement, mood and cognition. Furthermore, the PET scans for VMAT2 and glucose corresponded with each other, suggesting that the increase in dopamine may be one of the key mechanisms by which brain activity returns to normal after electrical stimulation, says Mills.
“We were able to see an increase in dopamine levels because we changed the way we looked at the problem,” says Mills. “Rather than looking at the amount of dopamine bound on receptors of dopamine-receiving cells, we looked at VMAT2 concentrations within dopamine-producing cells, which may be more sensitive to detecting changes in dopamine with deep brain stimulation in Parkinson’s disease patients.”
Smith and Mills both note that studies on more patients are needed to advance the search for better targets for electrical stimulation so that the brain produces more dopamine and patients reap additional benefits.
The researchers say that increasing dopamine through deep brain stimulation may even help them understand the applications to other psychiatric conditions. “In the long term we want to have a broader idea of the effects of electric stimulation on brain function and chemistry so that we can better treat Parkinson’s disease and other neurological and psychiatric conditions, like Tourette’s syndrome and depression, which are also affected by the dopamine system,” says Smith.
The research was supported by the NIH National Institute of Neurological Disorders and Stroke (NS101096), NIH National Institute on Aging (AG044441) and the Johns Hopkins Institute for Clinical and Translational Research (UL1TR001079).
Other contributors to the research include Greg Pontone, W. Stanley Anderson, Kate Perepezko, James Brasic, Yun Zhou, Jason Brandt, Daniel Holt, William Mathews, Robert Dannals and Dean Wong from Johns Hopkins, Christopher Butson from the University of Utah and Zoltan Mari from Cleveland Clinic.
DOI: doi.org/10.1016/j.parkreldis.2019.04.006
News release written by science writing intern Vandana Suresh for the Johns Hopkins Institute for Basic Biomedical Sciences.
