
Approximately one in 1000 pregnancies are complicated by neural tube defects, more commonly known as spina bifida. Postnatal surgery has been the most common management approach, but research has revealed that a prenatal procedure produces better results—both in the short and long term.
According to Michael Bebbington, MD, a Washington University Maternal-Fetal Medicine specialist, surgeon, and the Director of the Fetal Care Center at Barnes-Jewish Hospital and St. Louis Children’s Hospital, three primary benefits of this procedure have been identified—providing promise and hope for affected families.
- Reduction in the hindbrain herniation that typically accompanies an open neural tube defect. This herniation is responsible for the enlargement of the lateral ventricles inside the brain.
- Decreased risk of needing a shunt intervention to decompress the ventricles. If 80% of children who have neural tube defects need a shunt, that lowers to approximately 40% in children who undergo fetal surgery. Additionally, lack of a shunt equates to lack of shunt complications.
- Improvement in neurologic function. By closing over the exposed developing nerve tissue, the amount of damage that’s done in utero is lessened and neurologic function can be improved by up to two levels. For many kids, that means they will walk independently.
However, Dr. Bebbington warns this surgery is not appropriate for every case. “If there are other abnormalities, chromosomal abnormalities, or anything that would expose a mother to increased risk of prematurity like complex maternal medical conditions, they are not good surgical candidates,” he cautions. “In fact, we typically evaluate five or six families for every one family to which we offer the surgery.”
Pre- and Post-Surgical Expectations
To be considered, Dr. Bebbington and his team conduct a very thorough investigation during the mother’s evaluation visit. This visit is typically a two or three day event where women undergo a detailed ultrasound, fetal echocardiography, and fetal MRI.

Once a woman has been cleared for the procedure, the next steps are also intensive. Dr. Bebbington holds an extensive counseling session so families know what to expect and are fully aware of the risks. Families then meet with members from pediatric surgery, pediatric neurosurgery, neurology, and anesthesia departments.
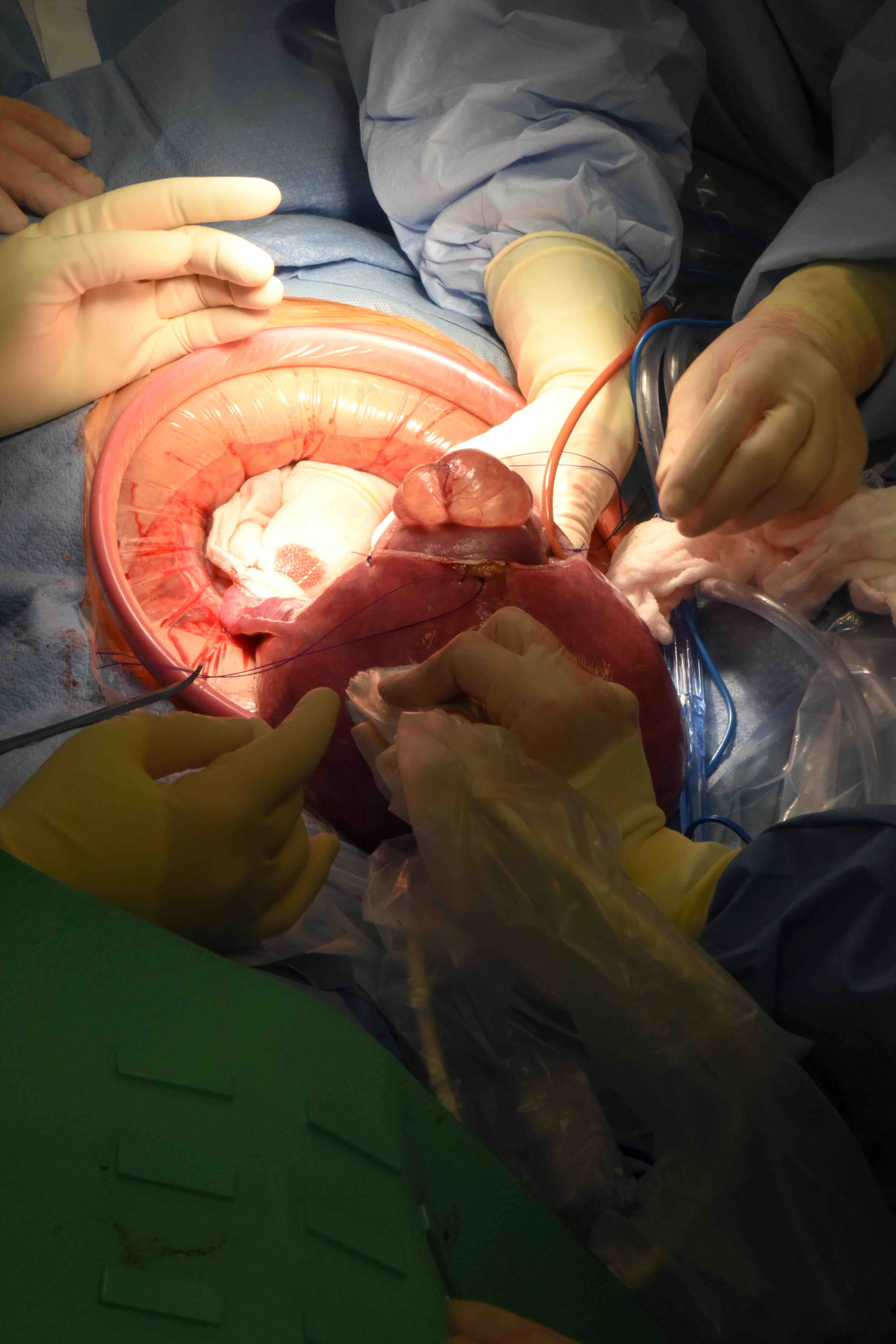
“Our goal is to provide perspective for the families on what the surgery involves so they go into this well informed about what they are undertaking,” states Dr. Bebbington. “It is a significantly major surgery—not only because we are opening the mother’s abdomen, but we are also opening the uterus to expose the baby’s back to allow closure of the defect. We then have to sew the uterus back up, make sure it’s a watertight seal, reinfuse amniotic fluid, and finally close the maternal abdomen.”
Pregnancy post-surgery is much different than a normal pregnancy. Mothers are on bed rest and must take medications to try to minimize the risk of preterm labor. Weekly follow-ups are also required until elective delivery occurs at 37 weeks.
“After women go through this surgery, they cannot go through labor,” explains Dr. Bebbington. “We ask them not to get pregnant again for at least a two-year period to allow for the uterine incisions to heal. Even after that, every pregnancy they have is at increased risk—not only for recurrence of spina bifida, but for increased risk of problems with the uterine scars.”
Dr. Bebbington advises women who do wish to become pregnant again to follow a strict folic acid regimen—but at a much higher dose than typical. “For a woman who has never had a pregnancy complicated by a neural tube defect, the amount of folic acid that’s sufficient to provide protection is approximately 400 micrograms. For a family that has had a pregnancy with a neural tube defect, the supplementation needs to be in the order of four milligrams.” As a result, the risk for recurrence is lowered by about 75%.
Don’t Wait to Seek Help
While the preventative step of maintaining one’s folic acid intake is highly effective, neural tube defects can still occur due to genetic abnormalities and epigenetic or environmental factors. Spina bifida can be detected as early as 12-14 weeks of gestation via ultrasound, but it is most commonly identified with a routine screening blood test called the maternal serum alpha-fetoprotein that’s typically done around 16 weeks. Once diagnosed, Dr. Bebbington encourages women not to wait to seek the help of a specialist.
“The best time to get a referral is as soon as it’s diagnosed,” he advises. “We can confirm that it is in fact an accurate diagnosis and then can have discussions with the family about what the best course of management might be.”
**To listen to an interview with Dr. Michael Bebbington, Washington University Maternal Fetal Medicine physician, surgeon, and Director of the Fetal Care Center, partnership between Barnes-Jewish Hospital, St. Louis Children’s Hospital and Washington University Physicians, follow this link: https://radiomd.com/stlouischildrens/item/39781
